The coronavirus SARS-CoV-2 pandemic has become a major global public health threat. In Africa, the virus spread seemed to be somehow delayed compared with Asia, Europe, and the USA.
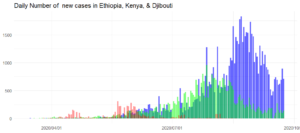
During the austral winter, the increase in transmission has accelerated on the African continent and one million cases were recorded as of August 07, 2020. In Ethiopia, COVID-19 cases are increasing rapidly. According to WHO report, as of September 23, 2020, Djibouti, Kenya, and Ethiopia had 5,407, 37,218, and 70,422 confirmed cases, and 61, 659, and 1,127 deaths, respectively. There is a need for decision-makers to have projections of the number of cases and its peak, and to be able to assess the impact of different interventions in local settings.
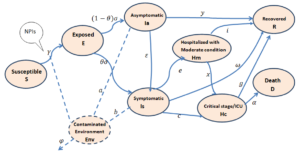
In the absence of a vaccine protecting against COVID-19, many countries have been implementing Non-Pharmaceutical Interventions (NPIs) to suppress or mitigate the disease spread. The known transmission pathways of COVID-19 to people are: i) close contact through respiratory droplets, ii) direct contact with infected persons, and iii) contact with contaminated objects and surfaces. Public health measures are intended to diminish those transmission mechanisms by implementing different mechanisms. In this project, the impact of face masking, hygiene and physical distancing will be assessed in Ethiopia, Kenya and Djibouti.
Mathematical modelling has been instrumental in the development of public health strategies to fight the COVID-19 in many countries (France, USA, China, UK, and Germany). We believe that, due to the difference in the age structure of the population, adherence to the enforced NPIs (face-masking, social-distancing, and hygiene), social interaction, and lifestyle in the Horn of Africa, mathematical models developed in other countries may not work to describe the disease dynamics there.
This project proposed a modified SEIR model (see Fig below) to predict the number of COVID-19 cases in different stages of the disease under different scenarios of NPIs implementation, with different adherence levels over time and distinguishing urban and rural settings in Djibouti, Kenya, and Ethiopia. Specifically, this project aims to:
i) develop a modified SEIR model and assess the impact of NPIs on the number of new cases in urban and rural settings in Ethiopia, Kenya, and Djibouti;
ii) assess how the implemented NPIs influence the size and peak time of the pandemic in the 3 Horn countries;
iii) estimate the number of subjects in each stage of the disease at the peak period in urban and rural areas of the three countries;
iv) provide recommendations to key stakeholders to control COVID-19.
Assessment of implemented and proposed intervention strategies for combating COVID-19, and predicting the number of new cases at different stages of the disease (i.e. asymptomatic cases, symptomatic cases, ICU cases), is a major challenge to both the public and scientific community. The outputs of this work will enable decision-makers in the Horn of Africa to choose efficient NPIs under different settings to mitigate COVID-19 and to prepare for temporary hospitals, medical facilities, and manpower in matching the number of cases predicted and its timeline.

